Case Summary 🔎
Patient Information
Age/Gender: 33-year-old
Systemic Condition: No underlying systemic disease, medically healthy
Clinical Findings
Tooth Site: Multiple sites
Diagnosis:
Recurrent caries on anterior abutment teeth
Severe inter-occlusal space deficiency due to progressive alveolar ridge resorption in the right partially edentulous maxilla
Radiographic Findings:
Extensive maxillary sinus pneumatization, resulting in minimal residual alveolar bone height insufficient for restoration
Clinical Summary
The patient returned 4 years after undergoing multiple retained root extractions and dental restorations. However, poor oral hygiene led to recurrent caries on the anterior abutments, requiring re-restoration.
Additionally, due to progressive alveolar ridge resorption in the right partially edentulous maxilla, inter-occlusal space was insufficient for proper restoration.
A portion of the residual ridge and gingiva needed to be removed, but this posed a risk of sinus membrane exposure due to severe maxillary sinus pneumatization.
Treatment Plan
Left-side sinus graft with a lateral approach, followed by an 8-month healing period
Implant placement after reduction of the inferior part of the residual bone
Conclusion
In this case, a sinus graft and crestal alveoloplasty were performed to secure inter-occlusal space for proper prosthetic restoration. Implants were successfully placed in the grafted bone, ensuring stable support for the final prosthesis.
The treatment outcome was excellent, and the patient achieved both functional and esthetic satisfaction.
Case Presentation
1️⃣ Pre-Op
The patient exhibited dental caries on #13 and #23 due to poor oral hygiene, with recurrent caries present beneath the crowns of the maxillary anterior teeth.
Additionally, extensive maxillary sinus pneumatization led to progressive downward resorption of the maxillary posterior edentulous ridge, while mandibular overgrowth further reduced inter-occlusal clearance, making prosthetic restoration challenging.
To address this, crestal alveoloplasty of the maxilla was planned following a sinus graft.
2️⃣ Surgery - Sinus Graft Lateral Approach (SLA)

Due to extensive pneumatization of the maxillary sinus and mandibular posterior ridge overgrowth, inter-occlusal clearance was insufficient, making prosthetic restoration challenging. Crestal alveoloplasty of the maxilla was planned following the sinus graft to address this issue.
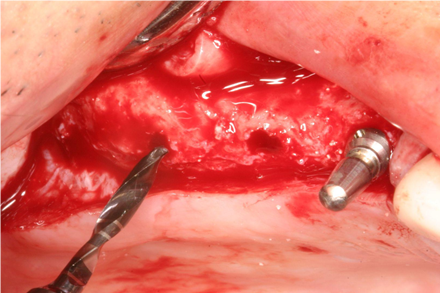
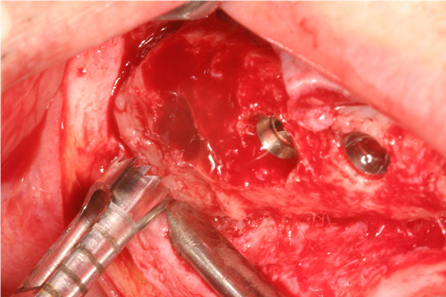
A small vertical incision was made, and the periosteum was elevated to expose the lateral wall of the maxillary sinus.
The LS-Reamer was used to create a lateral window, with careful depth control to prevent sinus membrane perforation. Within 30 seconds, the sinus membrane was successfully exposed without a bony disk.

The #02 elevator (90° angle) was used to detach the sinus membrane from the inferior lateral wall, followed by the #03 elevator (30° angle) to separate the membrane over the sinus floor.
For grafting, 2cc of DM bone (coral-based) and 2cc of Calpore were placed into the sinus cavity. The lateral window was then covered with a resorbable collagen membrane (Lyoplant) to protect the site.
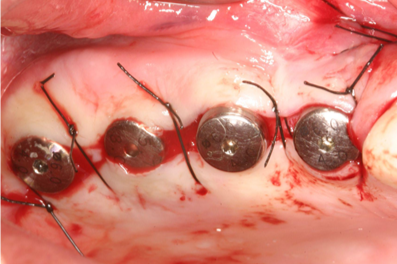
Simple interrupted sutures were placed along the vertical incision, and the site healed completely within 10 days, with no pain or swelling.
A postoperative panoramic radiograph showed a residual bone height of only 1mm. Crestal reduction of the alveolar ridge was planned 8–9 months later to create sufficient inter-occlusal space for restoration.

3️⃣ Surgery - Reduction Crestal-Alveoloplasty

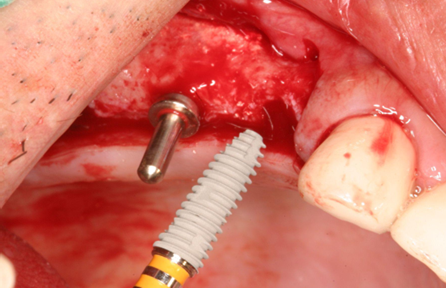
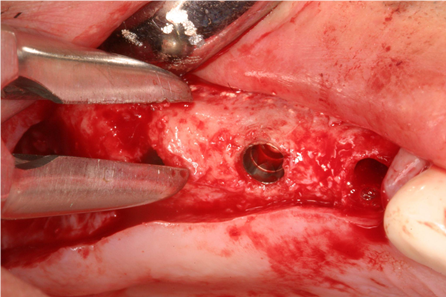
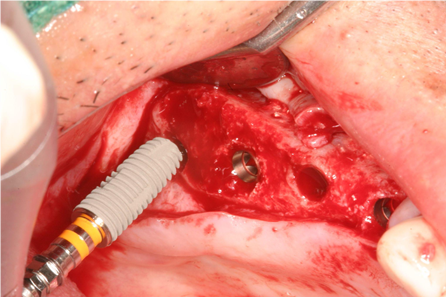
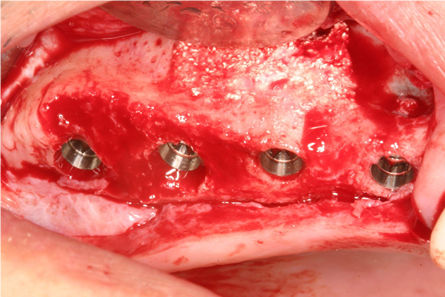
In the fully grafted site, four ∅5.0×13mm implants were successfully placed, as no residual bone remained. The lateral wall was completely filled with bone-like graft material, and an additional bone graft was performed at the apical area of implant #14 due to severe concavity.
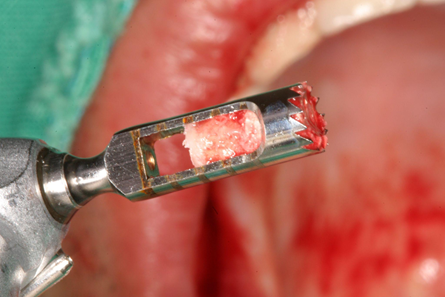
A trephine drill was used to harvest grafted bone from the third molar area (bone density: D3–2).
4️⃣ Post-Op
A panoramic radiograph taken 9 months post-graft confirmed well-corrected crestal bone levels and secured inter-occlusal space, ensuring a stable foundation for restoration.

A biopsy histology confirmed favorable bony remodeling around the graft material.
5️⃣ Final Restoration
The entire treatment took approximately 14 months to complete. A periapical X-ray at restoration delivery confirmed successful implant placement.

6️⃣ Follow-Up
A 2-year follow-up panoramic X-ray showed well-maintained marginal bone levels, with stable implants in the maxillary right posterior area, despite being supported only by grafted bone.