- Neo Biotech
- Aug 27, 2024
- 3 min read
Case Summary 🔎
Patient Information
Patient Information: 42 years old, Male
Medical History: Generally healthy, with normal blood pressure and no diabetes.
Chief Complaint(C.C): I want to have my removable denture changed to a fixed one.
Clinical Findings
Residual Bone Heights: Approximately 10mm, 4mm, and 6mm, with a concave-shaped sinus floor.
Treatment Plan
Case Presentation
1️⃣ Pre-Op
Pre-Op X-ray
2️⃣ Surgery: Sinus Lifting Procedures
After serial drilling with twist drills, S-reamers, specifically designed for sinus lift surgery, were used at a minimum of 1200 rpm. The process started by drilling 1mm short of the sinus floor depth, and then continued up to the opening of the inferior wall of the sinus.
S-reamer size for each implant
A periapical view after placing EB type CMI implant (4.0X11.5). The apex of the implant was placed 1-2mm into the sinus without bone graft (Class II CMI fixation) at #25 area. Bone density was D332 with 40 Ncm, which may be the result of obtaining Class II fixation.

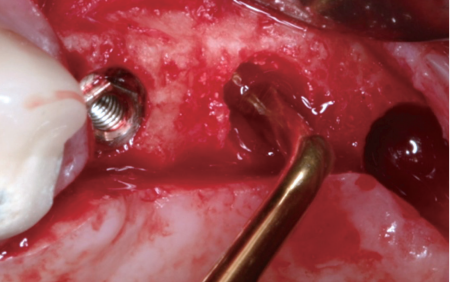
At #26 area, the available bone height was 3-4mm. The micro-elevators of the SLA kit were used to elevate the maxillary sinus membrane through the crestal hole. This procedure can be done in case of limited bone height (1-3mm).
0.3cc of alloplastic bone graft material (Calpore) was inserted below the elevated Schneiderian membrane to fill about 5mm at the #26 area.
Two EB type CMI implants (5.0X8.5) were placed at the #26 and #27 areas. Insertion torques were 40 and 30 Ncm at #26 and #27 respectively. That amount of insertion torque might result from a combination of inferior cortical fixation and selfcompaction technique.
Healing abutments were connected because of sufficient initial stabilities. Interrupted suture was performed with adequate attached gingiva.
3️⃣ Post-Op
Panoramic view right after surgery. About 7mm height of grafting material at the #26 fixture was observed as domeshaped radiopaque mass. It was possible to obtain extensive elevation with the micro-elevator.

4️⃣ Post-Op Follow-Up
1 month after implant placement surgery. Good soft tissue healing was seen. Impression was made at this time.
5️⃣ Final Prosthetics
A temporary cemented crown of #24 was removed. SCRP abutments were connected at #25, #26, and #27 one week after the impression.
A definitive SCR 3-unit PFM FPD (SCRP) was completed within 40 days after the surgery by cementing it on the abutments with a permanent resin cement. This prosthesis is retrievable through the screw holes.
After final prosthetics
6️⃣ Final X-ray
After final prosthetics
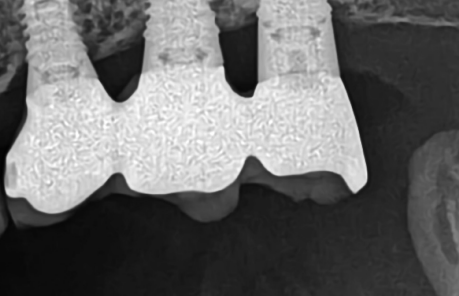
Panoramic view at prosthesis delivery shows stable marginal bone and elevated bone graft material.
Periapical radiograph shows no cement remnants at prosthesis delivery, due to SCRP type prosthesis which can be removed and polished separately. Good marginal fit between abutments and FPD is observed.
7️⃣ Follow-Up
3 year follow-up
A periapical view of 3 year follow-up. No specific difference was seen.
6 year follow-up
Panoramic view and a periapical view of 6 year follow-up. Peri-implant bone level is well maintained.
Occlusal view of the SCRP and CT images of #25, #26 and #27 implants at 6 year follow-up. Marginal bone levels were well maintained while 0.5mm of apices came out from the bone due to re-pneumatization, but were covered by the membrane. This may be a kind of bone remodeling phenomenon, explaining why no more bone is needed in the apex for occlusal support.
12 year follow-up
12 years later, during a follow-up, the prosthetic material had been changed from PFM to Zirconia, and the restoration was well-maintained with no signs of inflammation or marginal bone loss.
14 year follow-up
Intraoral photo and panoramic view of 14-year follow-up show stable marginal bone.